Understanding and Managing Discospondylitis in Dogs
Navigating Canine Spinal Health: Understanding and Managing Discospondylitis in Dogs
Key Takeaways
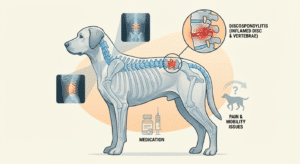
- Discospondylitis is a severe bacterial or fungal infection of a dog’s spinal discs and vertebrae, leading to pain and potential neurological damage.
- It often stems from infections elsewhere in the body (e.g., UTIs, dental disease) and is more common in large breeds and middle-aged to older dogs.
- Diagnosis relies on a combination of physical exams, X-rays, and advanced imaging like MRI, with tissue cultures being crucial for identifying the specific pathogen.
- Treatment is a long-term commitment, involving prolonged antibiotic or antifungal therapy (3-6 months), strict pain management, and sometimes surgery for severe cases.
- Early detection, diligent owner compliance with medication, and addressing underlying infections are vital for a good prognosis and preventing relapse.
Table of Contents
- What Is Discospondylitis in Dogs?
- Recognizing the Signs: Symptoms of Discospondylitis
- Diagnosis: Unraveling the Mystery
- Treatment: A Multi-faceted Approach
- Prognosis and Long-Term Management
- Prevention and Owner Awareness
- Connecting to Industry & Pet Wellness
- FAQ about Canine Discospondylitis
- Conclusion
The health and well-being of our canine companions are paramount, and staying informed about potential health challenges is a key part of responsible pet ownership. Among the various conditions that can affect dogs, spinal health issues often present unique diagnostic and treatment challenges. One such condition, crucial for every pet owner, veterinarian, trainer, and animal care professional to understand, is Discospondylitis in Dogs. This severe and often debilitating infection of the spine, specifically targeting the intervertebral discs and adjacent vertebral endplates, can significantly impact a dog’s quality of life if not diagnosed and managed promptly and effectively.
What Is Discospondylitis in Dogs?
At its core, discospondylitis is an inflammatory condition of the intervertebral disc and the vertebral endplates that border it, caused by an infection. As Kate Basedow, LVT, describes it, “Discospondylitis in dogs occurs when a bacterial or fungal infection travels to the spine. The infection might just be at one point in the spine or could be at multiple spots at once.” This succinct definition underscores the critical nature of the disease: it’s not simply a structural issue like a slipped disc, but an active, often aggressive, infection eating away at the very foundations of the spinal column.
The spine, a complex structure of vertebrae, intervertebral discs, and nerves, is vital for movement, support, and the protection of the delicate spinal cord. When an infection takes hold in this area, it can lead to pain, neurological dysfunction, and, if left untreated, irreversible damage. The infection typically reaches the spine via the bloodstream (hematogenous spread) from another site in the body. Common sources of these infections include urinary tract infections (UTIs), dental disease, skin infections, prostate infections, endocarditis, and even surgical procedures or trauma. Less commonly, fungal agents can be responsible, often stemming from environmental exposure or systemic fungal infections.
Understanding the mechanism of infection is key to both diagnosis and prevention. The intervertebral discs, lacking a direct blood supply in their central portion, are particularly vulnerable to infection once bacteria or fungi gain access to the highly vascularized endplates of the vertebrae. These endplates provide a fertile ground for microorganisms to multiply, leading to inflammation, bone destruction, and the characteristic lesions seen in discospondylitis. The infection can indeed be localized to a single disc space (focal) or spread to multiple areas along the spine (multifocal), making the clinical picture varied and sometimes challenging to pinpoint.
“Discospondylitis is often a secondary problem, a grim reminder that seemingly minor infections elsewhere in the body can have profound and devastating consequences if left unaddressed. It underscores the interconnectedness of a dog’s physiology and the importance of thorough veterinary care for even seemingly routine ailments.”— Dr. Eleanor Vance, Veterinary Internal Medicine Specialist
The Pathogens Responsible: Unmasking the Culprits
While a vast array of bacteria and fungi can cause discospondylitis, some culprits are more common than others.
- Bacteria:
- Staphylococcus aureus is the most frequently isolated bacterial pathogen, often originating from skin or urinary tract infections.
- Brucella canis is another significant bacterial cause, particularly in intact dogs. This bacterium is concerning not only for the dog’s health but also because it is zoonotic, meaning it can be transmitted to humans. Brucellosis often warrants specific diagnostic tests and treatment protocols.
- Other bacteria like Escherichia coli, Streptococcus spp., Klebsiella spp., and Pseudomonas spp. can also be implicated.
- Fungi:
- Aspergillus spp. and Coccidioides immitis (valley fever) are among the fungal organisms that can cause discospondylitis, especially in regions where these fungi are endemic. Fungal infections tend to be more challenging to treat and may require longer courses of antifungal medications.
Identifying the specific pathogen is critical because it directly influences the choice of antimicrobial therapy. Without a definitive diagnosis of the causative agent, treatment becomes empirical, which may or may not be effective, prolonging the dog’s suffering and potentially leading to resistance.
Who is At Risk? Predisposing Factors and Breeds
While any dog can potentially develop discospondylitis, certain factors increase the risk:
- Breed Predisposition: Large and giant breeds appear to be overrepresented, including German Shepherds, Boxers, Great Danes, Rottweilers, Doberman Pinschers, and Labrador Retrievers. The reasons for this predisposition are not fully understood but may relate to their physiology or higher incidence of certain predisposing conditions.
- Age: Middle-aged to older dogs (typically 3-7 years old) are most commonly affected, although discospondylitis can occur at any age, even in puppies.
- Immunocompromise: Dogs with weakened immune systems due to underlying diseases (e.g., Cushing’s disease, diabetes mellitus) or immunosuppressive medications are more susceptible.
- Previous Infections: Dogs with a history of recurrent urinary tract infections, dental disease, prostatitis, or endocarditis are at higher risk. Any unresolved systemic infection poses a threat.
- Trauma or Surgery: Spinal trauma or recent spinal surgery can create a portal for infection or compromise local immunity.
For breeders, understanding these predispositions is vital for monitoring their lines and educating potential owners. For pet owners, awareness of their dog’s breed and health history empowers them to be more vigilant.
Recognizing the Signs: Symptoms of Discospondylitis
The clinical signs of discospondylitis can be varied, insidious, and often overlap with other spinal conditions, making diagnosis challenging without a high index of suspicion. The primary symptom is pain, which can range from mild discomfort to excruciating agony.
Common symptoms include:
- Spinal Pain: This is the most consistent sign. Dogs may yelp when touched, show reluctance to be petted, or exhibit signs of discomfort when moving. The pain can be localized to the affected area or referred to other parts of the body.
- Reluctance to Move: Dogs may hesitate to jump, climb stairs, or get up and down. They might adopt a stiff, guarded posture.
- Lameness or Gait Abnormalities: Depending on the location of the infection, dogs might limp, drag their paws, or appear weak in one or more limbs (ataxia).
- Neurological Deficits: As the infection progresses and compresses the spinal cord or nerve roots, neurological signs can develop. These include:
- Weakness (paresis): Affecting one, two, or all four limbs.
- Paralysis (plegia): In severe cases, dogs may lose the ability to move their limbs entirely.
- Proprioceptive deficits: Difficulty knowing where their feet are in space, leading to stumbling or knuckling over.
- Incontinence: Loss of bladder or bowel control.
- Systemic Signs: These indicate a generalized infection and can include:
- Fever: Although not always present.
- Lethargy: Reduced energy levels, increased sleeping.
- Anorexia/Hyporexia: Loss of appetite or reduced food intake.
- Weight Loss: Due to chronic illness and reduced intake.
- Behavioral Changes: Dogs in chronic pain may become irritable, aggressive, or withdrawn. They might seek isolation or avoid interaction.
The progression of symptoms can be slow and subtle, often delaying veterinary attention until the disease is quite advanced. This is why vigilance and prompt veterinary consultation for any change in a dog’s gait, demeanor, or signs of pain are crucial.
“Many owners initially dismiss subtle signs like reluctance to jump or a change in activity level as just ‘getting old.’ However, with discospondylitis, early intervention is absolutely paramount. The sooner we identify the infection, the less likely we are to see irreversible neurological damage and the better the chances for a full recovery.”
— Sarah Chen, DVM, Board-Certified Veterinary Neurologist
Diagnosis: Unraveling the Mystery
Diagnosing discospondylitis requires a comprehensive approach, combining a thorough physical and neurological examination with advanced diagnostic imaging and laboratory tests.
1. Physical and Neurological Examination:
The veterinarian will carefully palpate the dog’s spine to identify areas of pain and assess the range of motion. A complete neurological examination is essential to localize any deficits, assess reflexes, and determine the severity of spinal cord compromise.
2. Imaging Studies:
These are the cornerstone of diagnosing discospondylitis.
- Radiographs (X-rays): Spinal radiographs are often the first imaging modality used. Early changes of discospondylitis, such as subtle bone lysis (destruction) and endplate irregularities, may not be evident for several weeks after the onset of infection. As the disease progresses, characteristic changes include:
- Narrowing or widening of the intervertebral disc space.
- Irregularity, sclerosis (hardening), and destruction of the vertebral endplates.
- New bone formation (osteophytes) bridging the affected vertebrae in chronic cases.
- Importance of serial radiographs: If initial X-rays are inconclusive but clinical suspicion remains high, repeat radiographs in 2-4 weeks may reveal clearer changes.
- Advanced Imaging (MRI or CT Scan): These modalities provide far greater detail than conventional X-rays, especially for visualizing soft tissues, the spinal cord, and nerve roots.
- MRI (Magnetic Resonance Imaging): Considered the gold standard for diagnosing discospondylitis. MRI can detect early inflammatory changes in the discs and vertebral endplates, visualize spinal cord compression, identify epidural abscesses (collections of pus outside the spinal cord), and help distinguish discospondylitis from other spinal conditions like disc herniation or tumors. It provides excellent soft tissue contrast.
- CT (Computed Tomography): Provides excellent bony detail and can be useful for evaluating the extent of bone destruction and sclerosis. While not as good for soft tissue as MRI, it can quickly identify significant bony lesions and spinal instability.
- Myelography: While less commonly used now due to the widespread availability of MRI, myelography (injecting contrast dye into the spinal canal) can outline the spinal cord and reveal areas of compression.
3. Laboratory Tests:
- Complete Blood Count (CBC) and Serum Biochemistry: These blood tests may reveal signs of systemic inflammation or infection, such as an elevated white blood cell count (leukocytosis), particularly neutrophilia, and increased inflammatory markers like C-reactive protein.
- Urinalysis and Urine Culture: Essential to identify a potential primary source of infection, especially if a UTI is suspected.
- Blood Cultures: If the dog is febrile or has signs of systemic illness, blood cultures can help identify the causative bacteria or fungi, though positive results are not always achieved.
- Brucella Serology: Absolutely crucial for intact dogs, and often recommended for all dogs with suspected discospondylitis, due to the zoonotic potential and specific treatment requirements of Brucella canis.
- Tissue Culture (Biopsy/Aspirate): This is the most definitive method for identifying the specific pathogen. Samples can be obtained via fine-needle aspiration or surgical biopsy of the affected disc space. This allows for bacterial and fungal culture and sensitivity testing, guiding the most appropriate antimicrobial therapy.
“While radiographs are a good starting point, we cannot overstate the value of advanced imaging like MRI. It allows us to visualize the intricate details of the spinal cord and surrounding structures, differentiate between infection and other pathologies, and plan the most effective course of treatment. This precision is a game-changer for patient outcomes.”
— Dr. Mark Davies, Diagnostic Imaging Specialist
Treatment: A Multi-faceted Approach
Treating discospondylitis is a long and often challenging journey that requires dedication from both the veterinary team and the pet owner. The primary goals are to eliminate the infection, manage pain, and restore neurological function.
1. Antimicrobial Therapy:
This is the cornerstone of treatment.
- Culture-Guided Therapy: Ideally, antibiotics or antifungals are chosen based on the results of bacterial/fungal culture and sensitivity testing from a tissue sample. This ensures the most effective drug is used against the specific pathogen.
- Empirical Therapy: If culture results are not available or are negative, broad-spectrum antibiotics are initiated. Common choices include cephalexin, clindamycin, or potentiated sulfonamides, often combined with fluoroquinolones, which have good bone penetration.
- Duration: Treatment is prolonged, typically lasting a minimum of 6-8 weeks, but often extending for 3-6 months or even longer, depending on the response to treatment, the pathogen, and the severity of the disease. Owner compliance with the full course of medication is absolutely critical to prevent relapse. Stopping antibiotics too soon is a common reason for recurrence.
- Fungal Infections: If a fungal cause is identified, specific antifungal medications (e.g., fluconazole, itraconazole) are used, often for many months, and can be quite costly.
2. Pain Management:
Dogs with discospondylitis are often in significant pain.
- NSAIDs (Non-Steroidal Anti-Inflammatory Drugs): Help reduce inflammation and pain.
- Gabapentin: An adjunctive medication often used for neuropathic pain.
- Opioids: May be used in the acute, severe pain phases.
- Strict Rest: Confining the dog to a crate or a small, enclosed space, with only short, leashed walks for elimination, is vital to prevent further spinal damage and reduce pain. This can last for several weeks or months.
3. Surgical Intervention:
Surgery is not typically the first line of treatment but is indicated in specific situations:
- Severe Neurological Deficits: If the spinal cord compression is severe and progressive, leading to significant neurological decline or paralysis, surgical decompression may be necessary to alleviate pressure on the spinal cord.
- Spinal Instability: If the infection has caused severe bone destruction leading to spinal instability, surgical stabilization may be required to prevent further damage and pain.
- Epidural Abscess Formation: Large collections of pus compressing the spinal cord may need surgical drainage and debridement.
- Failure of Medical Management: If the dog’s condition does not improve after an adequate course of antimicrobial therapy and pain management, surgery may be considered for definitive diagnosis (biopsy) and/or to address persistent infection or compression.
- Biopsy for Diagnosis: In cases where culture is critical and cannot be obtained non-invasively, surgery may be performed to collect a tissue sample.
4. Supportive Care and Rehabilitation:
- Nutrition: Maintaining good nutrition is essential for healing and immune function.
- Physical Therapy: Once the acute phase of pain and infection is controlled, physical rehabilitation can play a crucial role in restoring strength, mobility, and proprioception. This may include gentle massage, passive range of motion exercises, hydrotherapy, and therapeutic exercises.
- Monitoring: Regular re-evaluations, including repeat radiographs or advanced imaging, are crucial to monitor the progress of healing and ensure the infection is resolving. Blood tests may also be repeated to track inflammatory markers.
“Pet owners must understand that treating discospondylitis is a marathon, not a sprint. It demands unwavering commitment to medication schedules, strict activity restriction, and follow-up appointments. Patience and compliance are the most powerful tools in our arsenal against this insidious disease.”
— Emily Rodriguez, LVT, Canine Rehabilitation Specialist
Prognosis and Long-Term Management
The prognosis for dogs with discospondylitis is generally good to excellent, especially with early diagnosis, appropriate long-term antimicrobial therapy, and dedicated owner compliance.
- Factors Affecting Prognosis:
- Severity of Neurological Signs: Dogs with mild neurological deficits or pain tend to have a better prognosis than those with severe weakness or paralysis.
- Type of Pathogen: Fungal infections can be more challenging to treat than bacterial ones. Brucella canis infections also require specific considerations.
- Owner Compliance: Incomplete or premature discontinuation of medication is a major cause of treatment failure and relapse.
- Extent of Lesions: Multifocal lesions or severe bone destruction may indicate a more guarded prognosis.
- Relapse Potential: Even with successful treatment, there is a risk of relapse, especially if the primary source of infection is not identified and resolved, or if the antimicrobial course is too short. Lifelong vigilance for subtle signs is often recommended.
- Long-Term Monitoring: Regular veterinary check-ups and follow-up imaging are important to ensure complete resolution and monitor for any recurrence.
Prevention and Owner Awareness
While discospondylitis can strike unexpectedly, there are steps pet owners can take to minimize the risk and improve outcomes:
- Prompt Treatment of Infections: Any bacterial or fungal infection, no matter how minor it seems (e.g., ear infections, skin infections, UTIs, dental disease), should be treated promptly and completely under veterinary guidance.
- Spaying/Neutering: For intact dogs, particularly males, the risk of Brucella canis infection can be higher. Spaying or neutering reduces this risk and other associated reproductive health issues.
- Good Hygiene and Dental Care: Regular dental care, including professional cleanings, can prevent dental infections from spreading.
- Regular Veterinary Check-ups: Routine examinations allow veterinarians to identify and address underlying health issues before they escalate.
- Early Recognition of Signs: Being attuned to your dog’s normal behavior, gait, and activity levels means you can quickly spot any changes indicative of pain or discomfort and seek veterinary attention without delay.
- Preventing Trauma: While not always possible, minimizing activities that put excessive stress on the spine can be beneficial for at-risk breeds.
It’s Not Always the Most Wonderful Time of the Year (If You’re a Vet, Pet, or Pet Parent)
Connecting to Industry & Pet Wellness
The challenges posed by conditions like discospondylitis highlight several key areas of innovation and development within the broader pet industry, ultimately contributing to better pet wellness and care.
- Advanced Diagnostics: The increasing accessibility and sophistication of advanced imaging technologies like MRI and CT scans in veterinary medicine have revolutionized the diagnosis of complex conditions like discospondylitis. These tools allow for earlier, more accurate identification of spinal lesions, leading to timelier and more targeted treatment plans. For pet owners, this translates to better outcomes for their beloved companions; for veterinarians, it provides powerful diagnostic capabilities that enhance their practice; and for the pet industry, it fuels demand for specialized equipment, training, and veterinary imaging centers.
- Targeted Antimicrobials and Drug Development: Ongoing research in veterinary pharmacology aims to develop more effective antibiotics and antifungals with better penetration into bone and disc tissue, as well as reduced side effects. This innovation directly benefits pets by offering more potent weapons against stubborn infections and improving overall treatment efficacy.
- Veterinary Rehabilitation and Physical Therapy: The growth of veterinary physical therapy and rehabilitation as a specialized field has been instrumental in improving the recovery and quality of life for dogs recovering from spinal conditions, including discospondylitis. These services, offering hydrotherapy, therapeutic exercises, and pain management modalities, not only help dogs regain strength and mobility but also demonstrate the industry’s commitment to holistic pet care beyond acute treatment.
- Pet Insurance: The high cost associated with diagnosing and treating complex conditions like discospondylitis, which can involve expensive imaging, long-term medication, and potential surgery, underscores the growing importance of pet insurance. Pet insurance plans allow more owners to afford the best possible care for their pets, connecting a vital financial service to critical wellness outcomes.
- Veterinary-Client Communication and Education: The pet industry, including publications like this newsletter, plays a crucial role in educating pet owners about recognizing subtle signs of illness, understanding treatment protocols, and the importance of compliance. Empowered pet owners are better partners in their pet’s health journey, leading to improved outcomes for conditions requiring long-term management.
FAQ about Canine Discospondylitis
What is discospondylitis in dogs?
Discospondylitis is an infection of the intervertebral discs and the adjacent bones of the spine (vertebral endplates) in dogs. It is typically caused by bacteria or fungi that travel to the spine, often from another site of infection in the body.
What are the common symptoms of discospondylitis?
The most consistent symptom is spinal pain, which can manifest as reluctance to move, jump, or climb stairs. Other signs include lameness, gait abnormalities, weakness, paralysis in severe cases, fever, lethargy, loss of appetite, and behavioral changes due to chronic pain.
How is discospondylitis diagnosed?
Diagnosis involves a thorough physical and neurological exam, X-rays (radiographs), and often advanced imaging like MRI or CT scans for detailed visualization. Laboratory tests such as blood work, urinalysis, urine culture, blood cultures, Brucella serology, and tissue cultures from the affected area are crucial to identify the causative pathogen.
What is the treatment for discospondylitis?
Treatment primarily involves long-term antimicrobial therapy (antibiotics or antifungals) for 3-6 months or more, guided by culture and sensitivity results. Pain management, strict rest, and sometimes surgical intervention for severe neurological deficits or spinal instability are also essential components of treatment.
Can discospondylitis be prevented?
While not always preventable, the risk can be minimized by promptly treating all infections (e.g., UTIs, dental disease), spaying/neutering intact dogs, maintaining good hygiene and dental care, and regular veterinary check-ups to catch underlying health issues early. Early recognition of symptoms and swift veterinary attention are also key to better outcomes.
Elderly Cat’ Snuggles in Owner’s Jacket When Cold: A Deep Dive into Senior Pet Comfort and Care
Conclusion
In conclusion, discospondylitis in dogs is a serious but often treatable condition that demands awareness, early detection, and a committed approach to long-term veterinary care. By understanding its causes, recognizing its varied symptoms, embracing advanced diagnostic techniques, and adhering to comprehensive treatment plans, we can significantly improve the lives of dogs affected by this challenging spinal infection. As our knowledge of canine health continues to expand, fueled by dedicated research and innovation across the pet industry, the future holds promise for even more effective strategies in managing complex conditions and ensuring our loyal companions live their happiest, healthiest lives.

